In orthopedic trauma care, especially for elderly patients with osteoporotic bones, the Proximal Femoral Nail Antirotation (PFNA) has emerged as a game-changer for fixing proximal femur fractures. These are the types of fractures you often see in hip injuries, especially intertrochanteric fractures, the ones that happen between the neck and shaft of the femur. PFNA nail stands out because it doesn’t just fix the fracture; it stabilizes it in a way that lets patients get back on their feet faster. A big part of that success? Rotational stability.
So let’s break down how PFNA nails deliver on that front, without getting lost in dense medical jargon.
The Problem with Rotation
When someone breaks the top part of their femur, the pieces don’t just shift up or down—they rotate. That twist, especially in osteoporotic bone, makes healing harder and can lead to implant failure. Traditional fixation methods, like dynamic hip screws, don’t do a great job of controlling that rotation. The bone ends up moving slightly each time the person shifts weight, and over time, that can spell trouble.
What Sets PFNA Nail Apart?
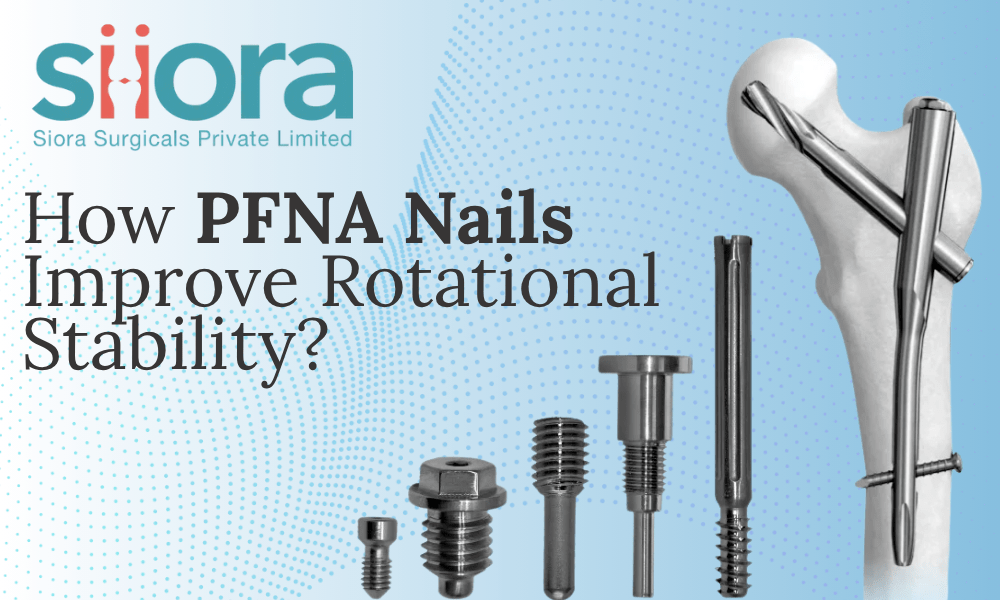
PFNA nails are intramedullary devices, which means they’re inserted into the hollow center of the bone. That alone gives them a mechanical edge—they sit closer to the body’s weight-bearing axis, so they handle forces more efficiently. But their real advantage comes from the helical blade.
The helical blade isn’t your typical screw. It’s designed to compact the bone around it as it’s inserted, rather than carving out space. This compaction does two big things:
- It creates a tight fit. The bone grips the blade from all sides, anchoring it firmly.
- It resists rotation. Since the blade isn’t just sitting loosely in a drilled-out tunnel, it doesn’t allow the femoral head to twist around it.
This matters most in osteoporotic patients. In softer bone, standard screws can strip out or allow micromovement. The PFNA’s helical blade, on the other hand, holds its ground.
A Locked System That Works Together
PFNA nails aren’t just about the blade. They’re part of a full system that locks the femoral head and shaft together. The helical blade is locked into the nail itself, meaning there’s no independent rotation at the joint. Think of it like welding two parts of a structure instead of bolting them loosely together; the entire setup moves as one solid unit.
This locked configuration is key for rotational stability. When the patient moves, the femur and the implant respond as one. There’s no twisting or shifting at the fracture site, which speeds up healing and reduces complications like implant migration or cut-out.
Real-World Impact
The result? Patients can start walking sooner, with less risk of the fracture shifting. In clinical studies, PFNA nails have shown lower rates of mechanical failure compared to traditional implants. They also reduce the chance of the femoral head collapsing or rotating, two common issues in hip fracture recovery.
For surgeons, PFNA nails mean fewer reoperations. For patients, it means a quicker return to independence.
Final Thoughts
PFNA nails aren’t magic, they’re just smart engineering applied to a common medical problem. By focusing on rotational stability through a compacting helical blade and a locked construct, they solve one of the key challenges in treating femoral fractures: keeping everything exactly where it needs to be while healing happens.
Learn about the technological advancements in the healthcare industry, including the orthopedic sector, by visiting the Florida International Medical Expo 2025.

Leave a comment